What is Autoimmune Disease?
Autoimmune disease is one of the most complex categories of health conditions, affecting millions of people worldwide.
The term 'autoimmune disorder' is also commonly used, and both refer to conditions where the immune system attacks the body’s own healthy tissues.
At its core, it occurs when the body’s own defense system—the immune system—malfunctions, and the body's ability to distinguish self from non-self is compromised, causing it to mistakenly attack healthy cells and tissues instead of protecting them.
This misdirected immune system activity creates chronic inflammation and organ dysfunction, often leading to lifelong health challenges.
At Daiwa Health Development, our focus on brain health, gut health, joint health, and functional wellness gives us a unique perspective on these conditions and how nutrition and supplements can support long-term management.
The Role of the Immune System
The immune system is designed to protect the body from harmful substances such as viruses, bacteria, and toxins. It has two main branches:
The innate immune system, often compared to frontline soldiers, responds quickly to any invader.
The adaptive immune system, or acquired system, provides specialized defenses, creating memory cells that recognize specific pathogens in the future.
When functioning correctly, this system knows to leave healthy cells untouched. But when immune system malfunctions occur, the body’s own defenses confuse self with non-self.
This misguided autoimmune response can cause severe tissue damage across many parts of the body, from the skin and joints to vital organs.
What Causes Autoimmune Disease?
The exact causes of autoimmune disorders remain unclear, but research supported by the National Institute of health and health and human services consistently highlights a combination of certain genes and environmental factors. Autoimmune diseases predominantly begin in adulthood, but they can start at any age.
Lifestyle elements such as diet, sleep, toxin exposure, and stress can trigger autoimmune disease in genetically predisposed individuals.
Studies in environmental health sciences also suggest that pollutants and infections may increase the risk of immune system attacks.
Factors That May Trigger Autoimmunity
- Genetics: Family history raises the risk of developing one autoimmune disease or even multiple.
- Environmental factors: Pollution, chemicals, and infections are well-documented triggers.
- Dietary influence: Gluten, for example, is linked to celiac disease and inflammatory bowel disease.
- Women’s health: Women face a higher risk, likely due to hormonal influences on t cells and thyroid hormone regulation. Women are more commonly affected by autoimmune diseases than men.
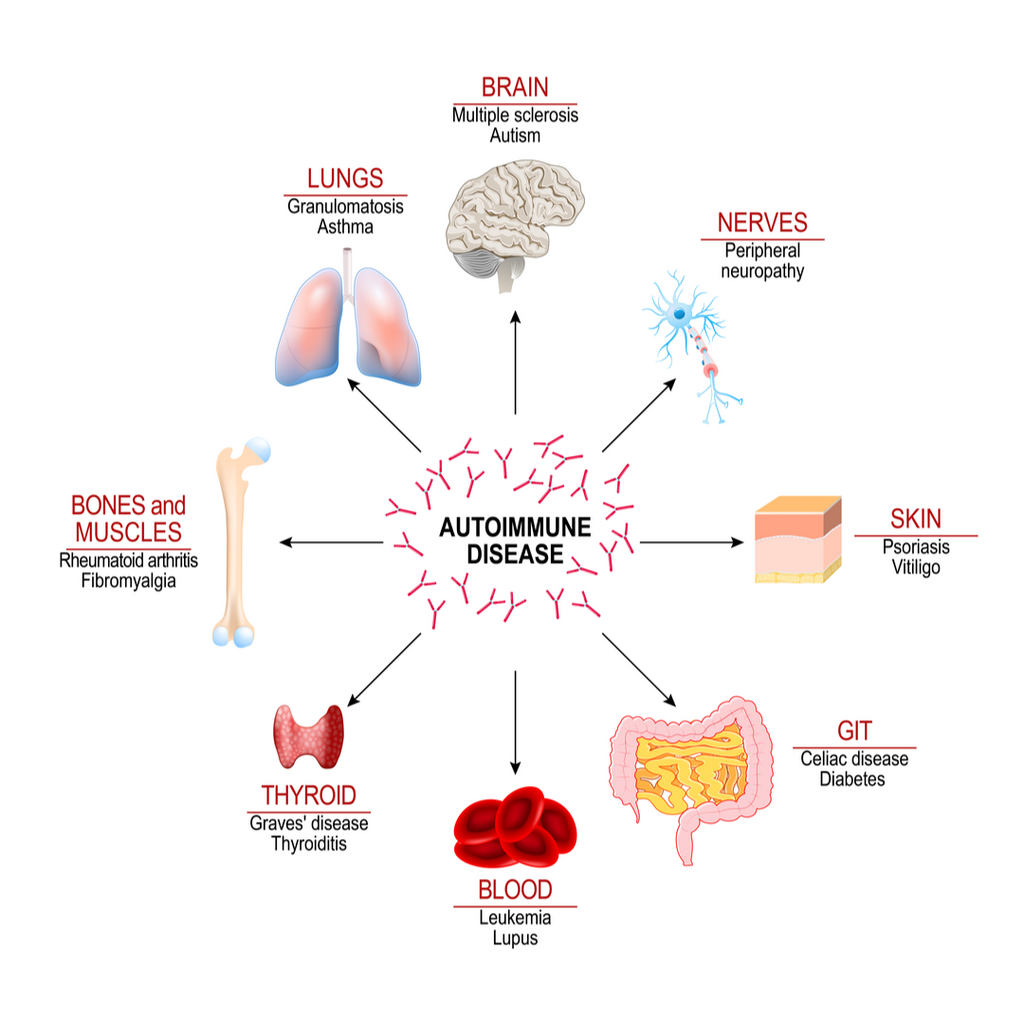
Types of Autoimmune Diseases
There are more than 100 recognized autoimmune diseases, each with unique targets but similar underlying mechanisms. Common autoimmune diseases include type 1 diabetes, multiple sclerosis, lupus, and rheumatoid arthritis.
The following sections will cover some of the most common diseases and their characteristics. While some affect specific organs, others involve multiple systems.
Endocrine-Related Disorders
- Type 1 diabetes: The immune system attacks insulin producing cells in the pancreas, disrupting the body’s ability to regulate blood sugar.
- Hashimoto’s thyroiditis: The most common thyroid-related autoimmune condition, where the thyroid gland becomes underactive due to chronic inflammation.
- Graves disease: The opposite process, leading to excessive thyroid hormone production.
Rheumatologic Conditions
- Rheumatoid arthritis: A hallmark example where the immune system attacks the joints, causing swelling, stiffness, and long-term damage.
- Systemic lupus erythematosus: A systemic condition with varied lupus symptoms such as skin rashes, fatigue, and joint pain.
- Sjögren’s syndrome: An autoimmune disorder characterized by dry eyes, dry mouth, and joint pain. Sjögren's syndrome is often associated with other autoimmune conditions and can extend to lung and kidney involvement.
Neurologic Disorders
- Multiple sclerosis: Here, the immune system attacks the protective sheath around the spinal cord and central nervous system, leading to muscle weakness, tingling, and mobility issues.
- Guillain Barre syndrome: A rare but serious attack on the nervous system, often following infection.
Gastrointestinal and Dermatologic Diseases
- Inflammatory bowel disease, including ulcerative colitis and Crohn’s disease, causes chronic inflammation of the digestive tract, often accompanied by abdominal pain and extra-intestinal symptoms.
- Psoriasis: An attack on skin cells causing itchy, scaly plaques.
- Alopecia areata: Involves patchy hair loss due to immune activity in hair follicles.
Blood Vessel Involvement in Autoimmune Disease
Blood vessel involvement is a significant aspect of many autoimmune diseases, as the immune system’s misguided attacks can lead to inflammation and damage within the blood vessels themselves.
This process, known as vasculitis, can cause a variety of symptoms depending on which vessels and organs are affected.
For instance, in rheumatoid arthritis, inflammation can extend beyond the joints to impact blood vessels, sometimes resulting in narrowed or weakened vessels that may contribute to joint pain, skin rashes, or even abdominal pain.
Systemic lupus erythematosus is another autoimmune disease known to affect blood vessels, potentially leading to symptoms such as unexplained weight loss, fatigue, and more severe complications if organ blood supply is compromised.
Because blood vessel involvement can affect many parts of the body, early recognition and management are crucial.
Treatment often includes anti-inflammatory medications and immunosuppressants, alongside lifestyle changes like regular exercise and smoking cessation, to help protect vascular health and reduce the risk of further complications.
Diagnosing Autoimmune Conditions
Because similar symptoms occur across conditions, diagnosis is challenging. Doctors rely on a combination of health history, physical exams, imaging, and blood tests. Diagnosing autoimmune diseases can be challenging due to their diverse presentations and transient symptoms. Common markers include:
- Autoimmune antibodies such as ANA in lupus or rheumatoid factor in rheumatoid arthritis.
- Abnormal hormone levels, such as low thyroid hormone in Hashimoto’s thyroiditis.
- Specialized antibody testing for conditions like celiac disease.
No single test confirms every case. For this reason comprehensive evaluation by a healthcare professional is essential.
Can You Live a Long Life with Autoimmune Disease?
Yes—many individuals with autoimmune disorders live long, fulfilling lives. Treatments aim to manage symptoms, protect organ function, and reduce flare-ups. Medical care often includes medication, physical therapy, and in severe cases, blood transfusions for conditions affecting blood cells or red blood cells. Corticosteroids are commonly used to treat autoimmune diseases by suppressing the immune system.
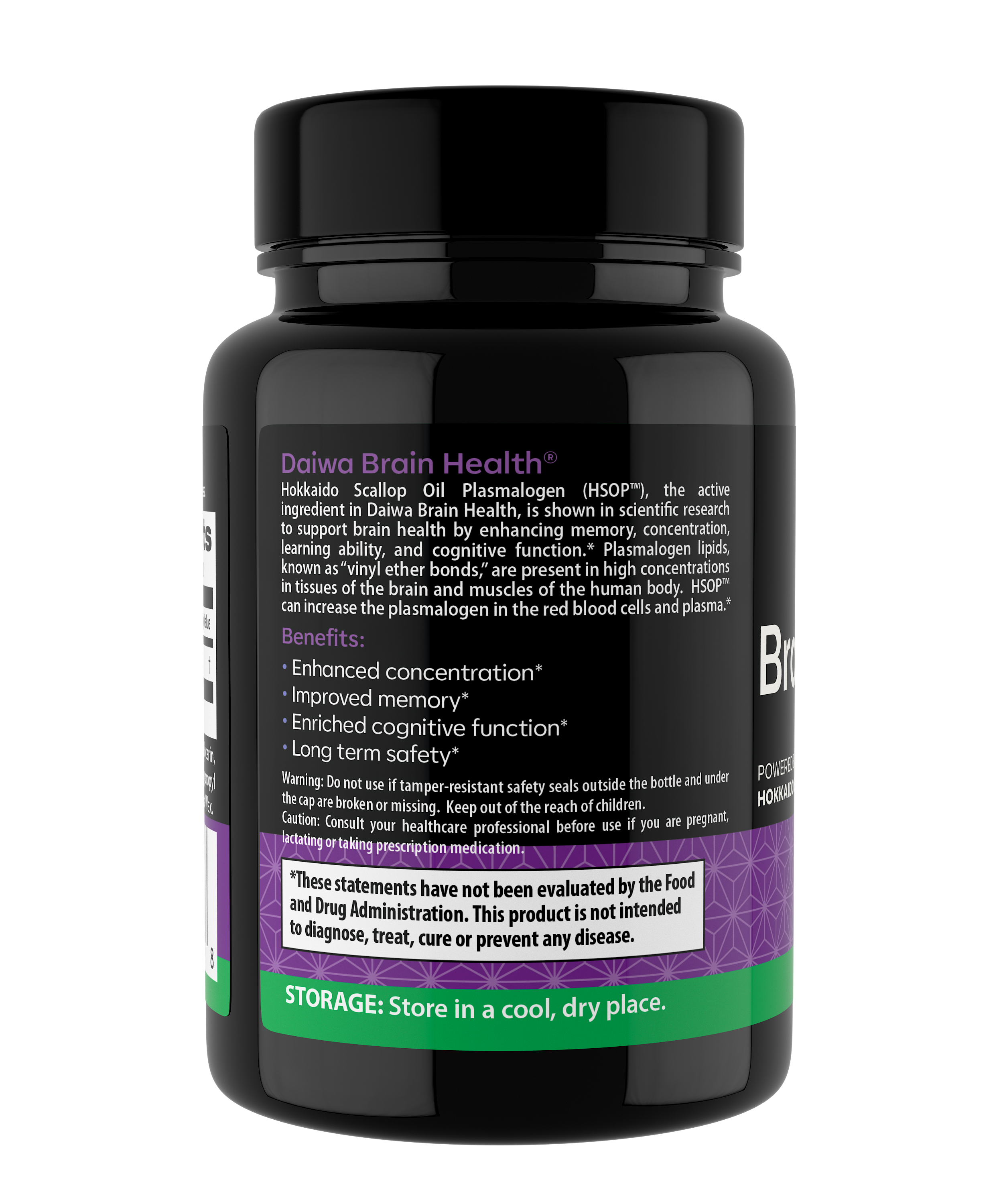
Complementary strategies—such as stress reduction, diet improvement, and supplement support—can enhance resilience. Daiwa Health Development emphasizes functional medicine tools like vitamin D optimization, gut support, and targeted supplements to reinforce the body’s natural balance.
Managing and Supporting Autoimmune Health
Traditional treatments control inflammation, but integrative strategies improve quality of life. Key approaches include:
- Nutritional support: Healthy inflammatory diets can reduce flares in inflammatory bowel disease and improve women’s health outcomes in thyroid conditions.
- Stress management: Chronic stress worsens immune system activity and can trigger autoimmune disease flares.
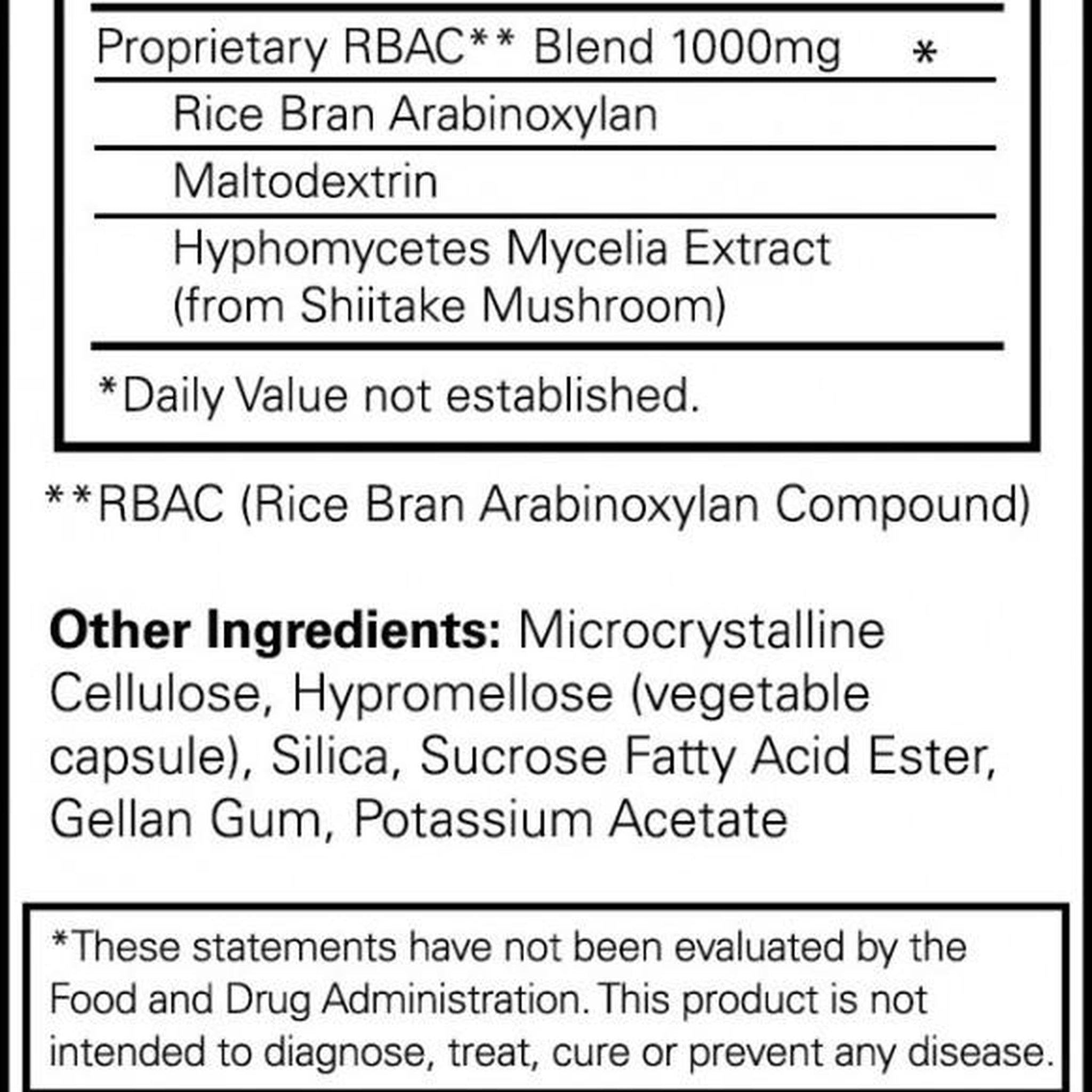
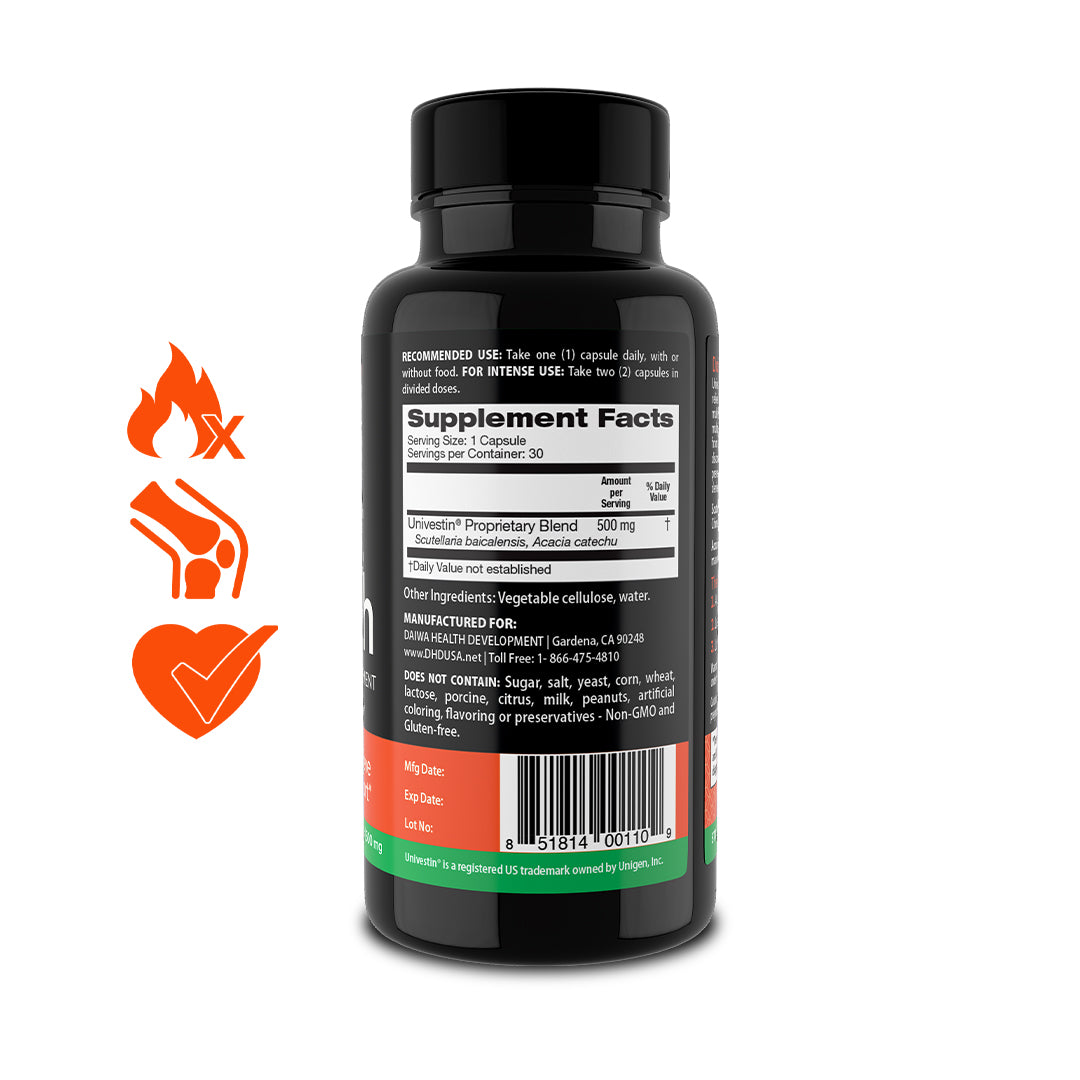
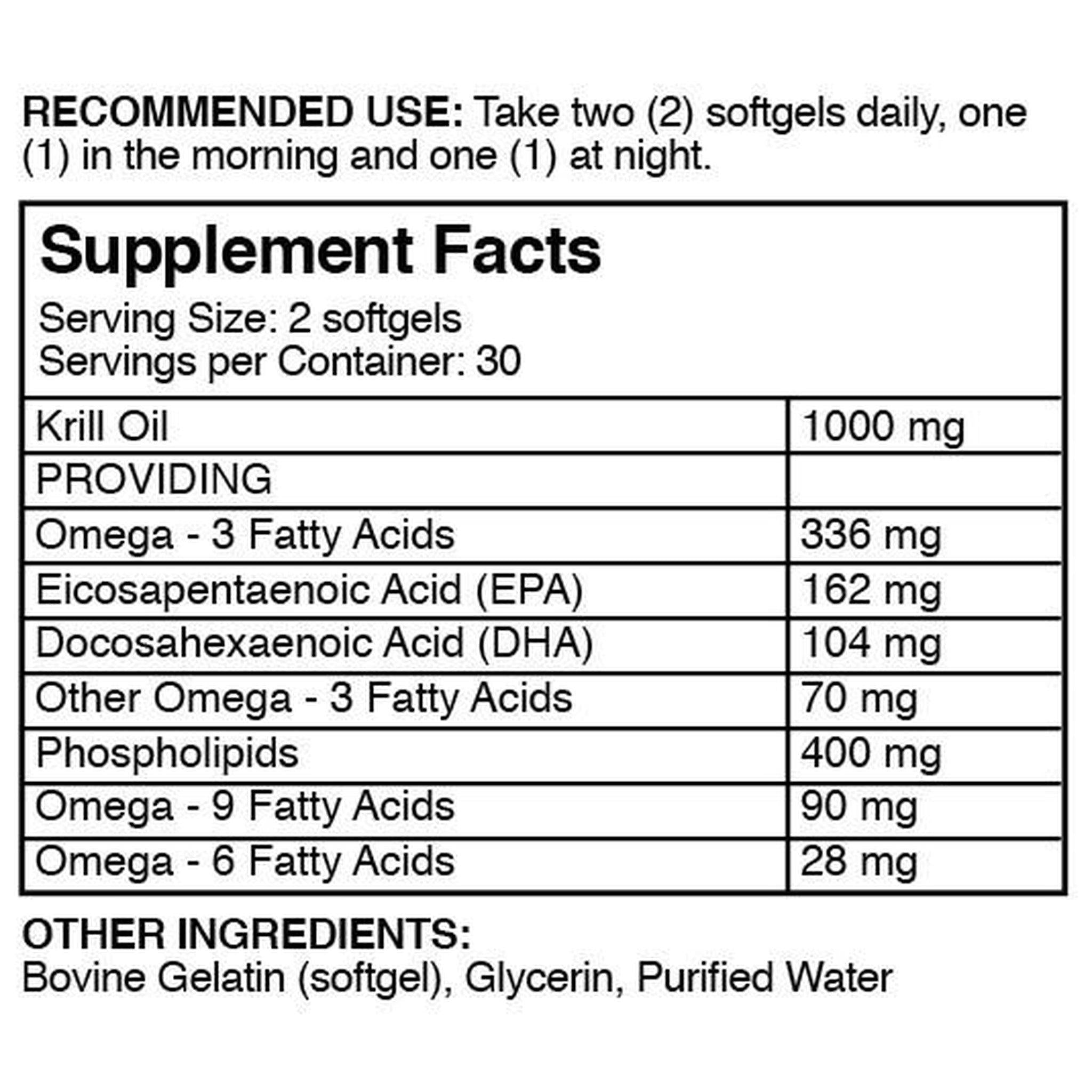
- Supplementation: At Daiwa Health Development, our supplements are designed to optimize gut and brain health, supporting the immune system, as immune modifiers, without overstimulation.
- Movement and therapy: Gentle exercise, physical therapy, and adaptive strategies help counter muscle aches and stiffness.
Mental Health Considerations in Autoimmune Disease
Living with an autoimmune disease can take a toll not only on the body but also on mental health. Many people with autoimmune diseases experience challenges such as depression, anxiety, and emotional distress, which can be triggered by the chronic nature of the illness, unpredictable symptoms, and the impact on daily life.
For example, individuals with multiple sclerosis may face heightened anxiety or depression due to the uncertainty of flare-ups and the effect of symptoms on their independence and activities. Addressing mental health is an essential part of comprehensive autoimmune disease care.
Supportive strategies may include counseling or therapy, medication when appropriate, and lifestyle adjustments like stress management techniques and building a strong social support network. Recognizing and treating mental health symptoms early can greatly improve overall well-being and quality of life for those affected by autoimmune conditions.
Family Planning and Autoimmune Disease
Family planning is an important consideration for individuals with autoimmune diseases, as certain conditions can increase the risk of pregnancy complications and may affect both maternal and fetal health. Women with systemic lupus erythematosus, for example, are at a higher risk for complications such as preeclampsia and preterm labor, while those with rheumatoid arthritis may face increased risks of gestational diabetes and hypertension.
Planning for pregnancy with an autoimmune disease often involves preconception counseling to assess risks and optimize health, as well as close monitoring throughout pregnancy by a multidisciplinary healthcare team, including an obstetrician and a rheumatologist. With careful planning and medical support, many women with autoimmune diseases can achieve healthy pregnancies and positive outcomes for both mother and baby.
Work-Related Issues and Autoimmune Disease
Autoimmune diseases can present unique challenges in the workplace, as symptoms like joint pain, fatigue, and muscle weakness may impact job performance and daily functioning. For example, individuals with rheumatoid arthritis may find it difficult to perform tasks that require fine motor skills or prolonged standing, while those with multiple sclerosis might experience cognitive changes or muscle weakness that affect their ability to work efficiently. Addressing work-related issues often involves a collaborative approach, including workplace accommodations such as flexible schedules, ergonomic modifications, and assistive devices. Support from healthcare professionals, such as occupational therapists and vocational rehabilitation counselors, can help individuals with autoimmune diseases navigate employment challenges, maintain productivity, and protect their health.
National Institutes and Research Initiatives
Ongoing research by national institutes is vital for advancing our understanding of autoimmune diseases and improving treatment options. Organizations like the National Institute of Environmental Health Sciences (NIEHS) are investigating how environmental factors, such as exposure to toxins and pollutants, can trigger autoimmune disease in susceptible individuals. The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) focuses on the causes and management of autoimmune diseases like rheumatoid arthritis and lupus, while the National Institute of Neurological Disorders and Stroke (NINDS) leads research into neurological autoimmune conditions, including multiple sclerosis and Guillain-Barré syndrome. These national institutes and their research initiatives play a crucial role in uncovering the underlying mechanisms of autoimmune diseases, developing new therapies, and ultimately improving the lives of those affected.
Living Well with Autoimmune Disease
Although there is no universal cure, people with many autoimmune diseases can thrive through a holistic approach. Research from the Cleveland Clinic and Boston Children’s Hospital highlights the importance of personalized care, early intervention, and lifestyle adaptation. Recognizing early common symptoms such as fatigue, rash, or swelling allows faster management and better outcomes.
Pro Tip: Partner with a healthcare professional who understands the integrative model. This partnership ensures medical treatment is balanced with functional medicine, nutritional strategies, and safe supplementation.
Conclusion: Building a Healthier Future
So, what is autoimmune disease? It is a complex imbalance where the body’s immune system turns against its own tissues, driven by genetics, lifestyle, and environmental factors. While challenging, these conditions are not without hope. With targeted therapies, functional nutrition, and supplement support, individuals can regain control over their health. At Daiwa Health Development, we believe in science-backed supplements that help restore balance in brain, gut, joint, and overall wellness—empowering individuals to live healthier lives despite the challenges of autoimmune conditions.












Wow. This is very useful information!