Excess Salt and Inflammation

Salt is everywhere. It’s in the shaker on your table, in restaurant meals, and hiding in packaged foods at the grocery store. For centuries, salt has been prized for flavor and preservation, and for good reason—it keeps food safe and makes meals taste satisfying. The body also depends on it for essential functions.
But here’s the catch: while we need a little, we don’t need much. The modern diet contains far more sodium than our bodies are built to handle. Over time, this overload causes problems. Excess salt and inflammation are directly linked, creating ripple effects that show up as high blood pressure, heart disease, kidney strain, and flare-ups in autoimmune conditions.
At Daiwa Health Development, we’ve seen firsthand how health can change when people take sodium seriously. Lifestyle adjustments, paired with supplements that support the body’s natural defenses, can make the difference between chronic symptoms and lasting wellness.
Why Salt Is So Important
Salt is more than seasoning. The chemical compound sodium chloride—better known simply as salt—has a central role in the body. Sodium helps nerves send messages, supports muscle contraction, and balances the amount of water inside and outside cells. Without it, basic systems would fail.
Yet balance is everything. The same sodium that keeps the body running smoothly becomes a burden when salt intake goes beyond what’s needed. That excess is what damages blood vessels, pushes blood pressure higher, and increases the risk of cardiovascular disease. High salt consumption can also impact calcium loss from bones, further contributing to long-term health risks.
The World Health Organization estimates that the average daily sodium intake worldwide is about 3,400 mg. Compare that to the recommended dietary guidelines of 2,300 mg per day, and you’ll see the gap. Most Americans consume about 3,400 mg of sodium per day, exceeding recommended limits. For some patients, especially those already living with hypertension or kidney disease, 1,500 mg per day is a safer limit.
Too much sodium isn’t just a number on paper—it translates into measurable risks for the heart, kidneys, and immune system.
Salt and the Immune System
When sodium levels rise in the blood, they don’t just change fluid balance—they change how immune cells behave. Excess salt can also alter mitochondrial function, which plays a critical role in energy production and cellular health, further compounding its effects on the body.
Research shows that a high salt diet leads to the production of more reactive oxygen species (ROS). These unstable molecules create oxidative stress, which damages cells and tissues. That stress then sparks the release of proinflammatory cytokines such as IL-6, chemical messengers that keep inflammation alive in the body.
It doesn’t end there. Salt also causes cytoskeletal rearrangement in T cells, altering their structure and making them more reactive. This heightened state can push the immune system into overdrive, leading to stronger inflammatory responses.
For patients already dealing with autoimmune diseases like rheumatoid arthritis or systemic lupus erythematosus, too much salt often means worsening symptoms. Flares become more frequent, pain increases, and quality of life decreases. Studies in both humans and animal models show that sodium plays a crucial role in immune responses, far beyond its impact on blood pressure.
Can Too Much Salt Really Cause Inflammation?
The answer is yes.
Excess salt disrupts the body’s delicate balance. Instead of supporting immune cells in their normal work of protecting against infection, it drives them toward producing more reactive oxygen species and releasing proinflammatory cytokines. This chain reaction doesn’t stop—it builds.
Over time, this heightened state of inflammation contributes to:
- Autoimmune disease flare-ups
- Atherosclerosis, where arteries harden and narrow
- Insulin resistance, which raises the risk for type 2 diabetes
Humans simply aren’t designed to process excessive amounts of sodium chloride every day. Historically, diets were lower in sodium, relying on fresh, whole foods. Today, processed and restaurant meals dominate, and sodium content has climbed with them. This shift in eating habits explains why chronic diseases linked to inflammation are on the rise.
How the Body Signals Too Much Salt
Inflammation is often invisible. But the body does send signals when salt intake has climbed too high:
- Swelling or puffiness, caused by water retention.
- Persistent thirst, as the body works to dilute sodium levels.
- Headaches, tied to fluid imbalances and blood pressure shifts.
- Fatigue, when the cardiovascular system is working overtime.
These symptoms don’t always get linked back to sodium intake right away. But together they show how much salt weighs on the body’s natural balance.
Impact on Kidneys and the Heart
The kidneys are the body’s natural filter. Their job is to regulate sodium and remove excess through urine. When sodium intake is moderate, they handle it. But when salt intake remains high day after day, the kidneys can’t keep up.
As a result, the body holds onto water to dilute sodium in the blood. That means blood volume increases, which pushes blood pressure higher. This condition, known as hypertension, is one of the most well-documented effects of excess sodium.
Over time, hypertension forces the heart to adapt. The heart muscle thickens in a process called left ventricular hypertrophy. While this may seem like a way to cope with the added pressure, it actually makes the heart less efficient and more prone to failure.
Another outcome is fluid buildup around the heart and lungs, which places additional stress on the cardiovascular system. Together, these changes pave the way for heart disease, stroke, and kidney disease—three of the most serious outcomes of excess sodium.
Evidence from Research
Research has made it clear: sodium has consequences.
- A cross sectional study published in Public Health Nutr found that regions with high salt consumption also had higher rates of hypertension and cardiovascular disease.
- Human studies show that sodium chloride increases the production of inflammatory cytokines and damages blood vessels.
- Animal models confirm that high sodium diets alter immune responses, triggering inflammation that mirrors human conditions.
Authors declare that sodium plays a central role not just in regulating blood pressure but in fueling the processes behind chronic inflammation and disease.
How Much Salt Is Too Much?
The reality is that most people are eating more salt than they realize. Even those who rarely pick up a salt shaker often exceed limits because sodium hides in processed foods, sauces, condiments, and restaurant meals. Nearly all canned and ready-made convenience foods contain sodium, making it challenging to stay within recommended limits without careful planning.
Here’s what experts recommend:
- Dietary guidelines: no more than 2,300 mg of sodium per day for healthy adults.
- Lower targets: 1,500 mg per day for patients with high blood pressure, kidney disease, or autoimmune disease. Adults over 51 years old, African Americans, and those with high blood pressure, diabetes, or kidney disease should also aim for this lower sodium intake.
- Awareness: checking labels and portion sizes can reveal just how much sodium is sneaking in.
A low sodium diet doesn’t mean flavorless meals. Herbs, spices, citrus, and whole food ingredients bring natural flavor without the added sodium load. Pairing these foods with vegetables, whole grains, and lean proteins not only reduces sodium but actively supports blood vessel health and lowers systemic inflammation.
Pro Tip: Flushing Out Excess Sodium
It happens—we all have days when sodium intake is higher than it should be. The good news is there are ways to help the body restore balance:
- Drink more water: hydration helps kidneys remove sodium more efficiently.
- Eat potassium-rich foods: bananas, sweet potatoes, and leafy greens help counterbalance sodium.
- Move your body: exercise and sweating naturally lower sodium levels.
- Choose whole foods: cutting back on processed items reduces sodium intake without guesswork.
Think of it as giving the body a reset. Even a single day of excess salt intake can be offset with conscious choices the next.
Why Eating Habits Are the Real Driver
It’s not the salt shaker that’s causing trouble. It’s the foods we rely on daily. More than 70% of sodium intake comes from packaged, processed, or restaurant meals. That means the easiest way to cut back is to shift eating habits.
Instead of fast food, reach for meals built on whole grains, fresh vegetables, and lean proteins. Instead of salty snacks, keep fruit, nuts, or unsalted options on hand. By making gradual swaps, patients reduce their sodium load and give their bodies a better chance at long-term disease control.
For patients with rheumatoid arthritis, lupus, or other autoimmune diseases, this shift can be especially powerful. Many report fewer flare-ups and improved energy on a low sodium diet. It’s proof of how much salt sensitivity can influence the immune system.
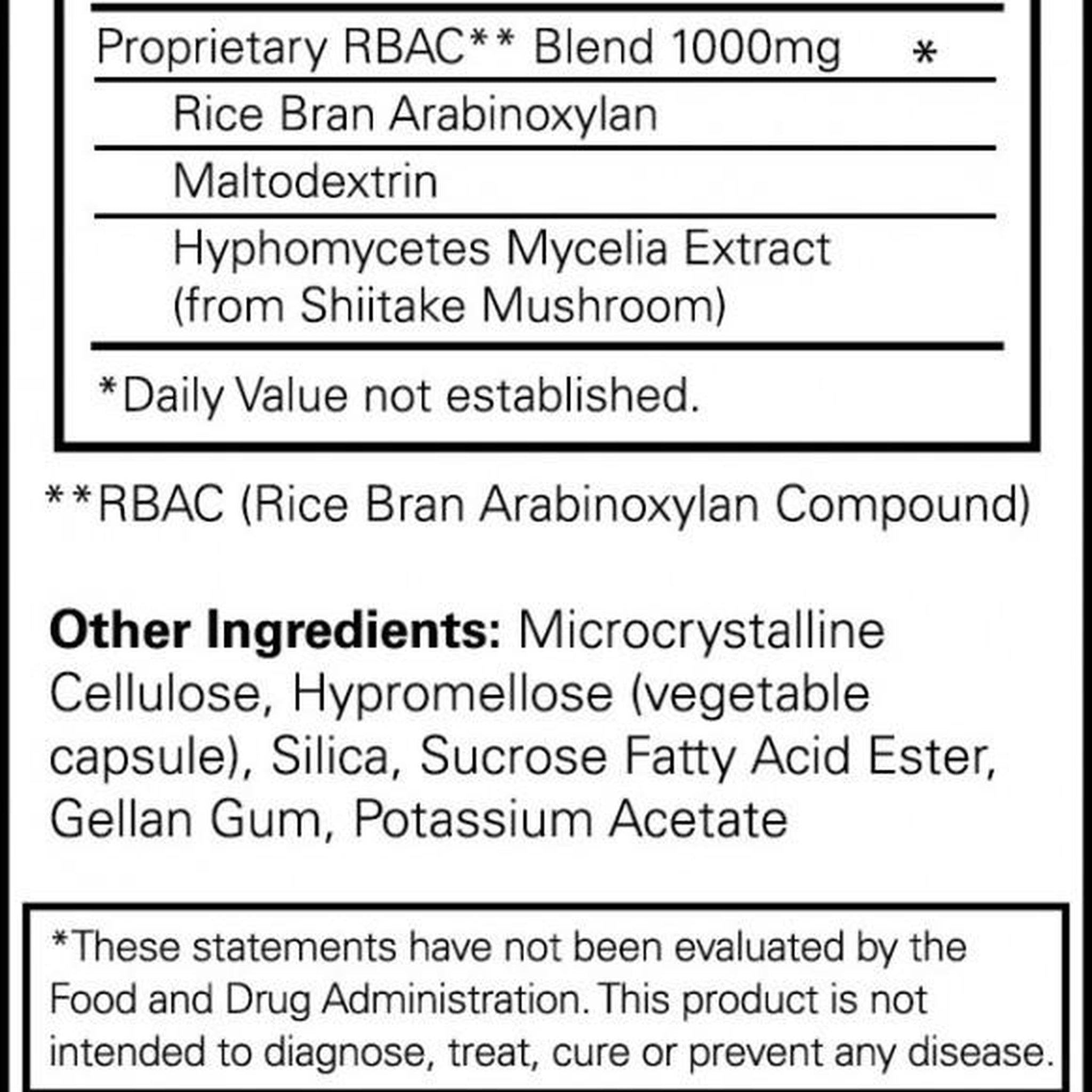
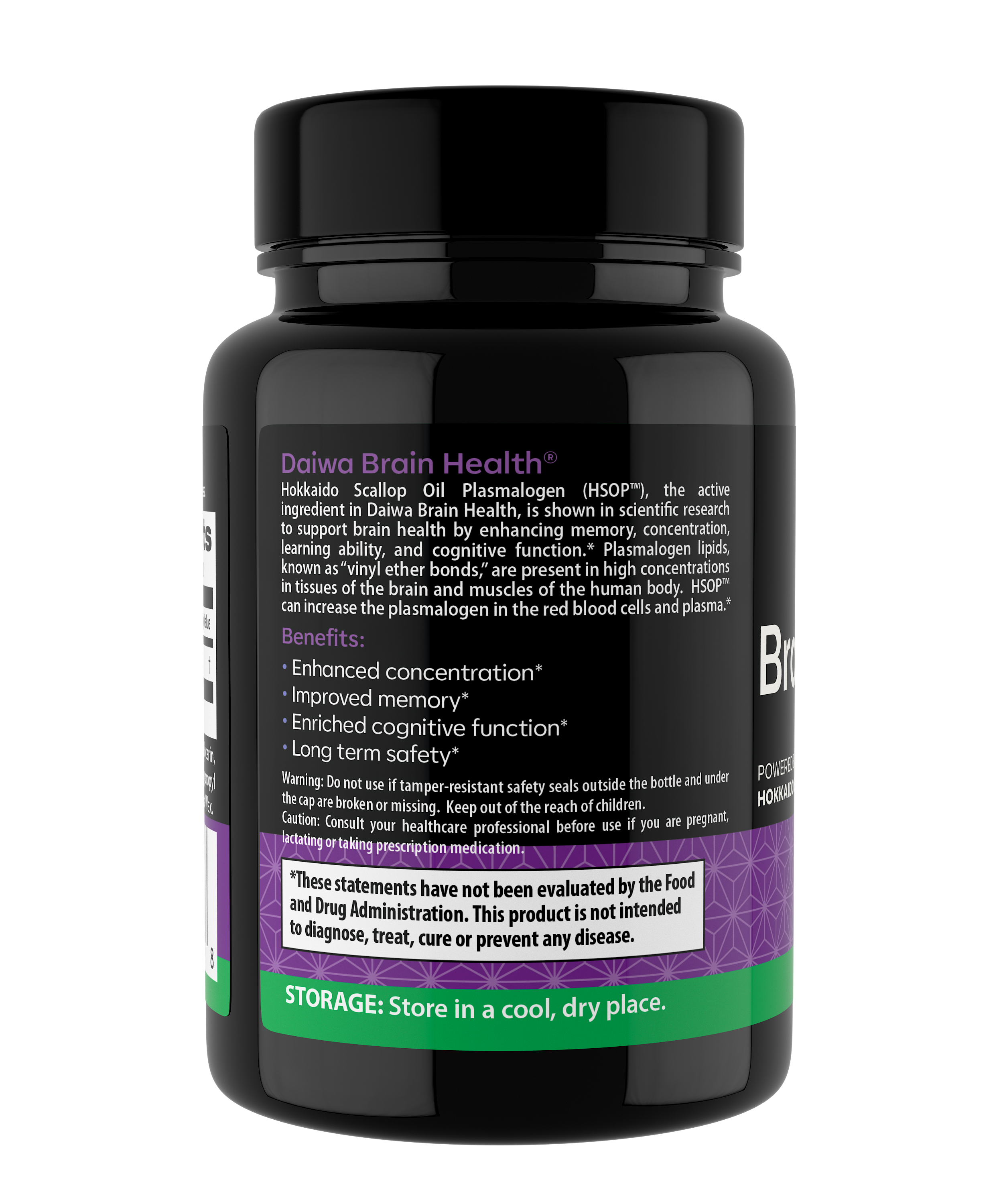
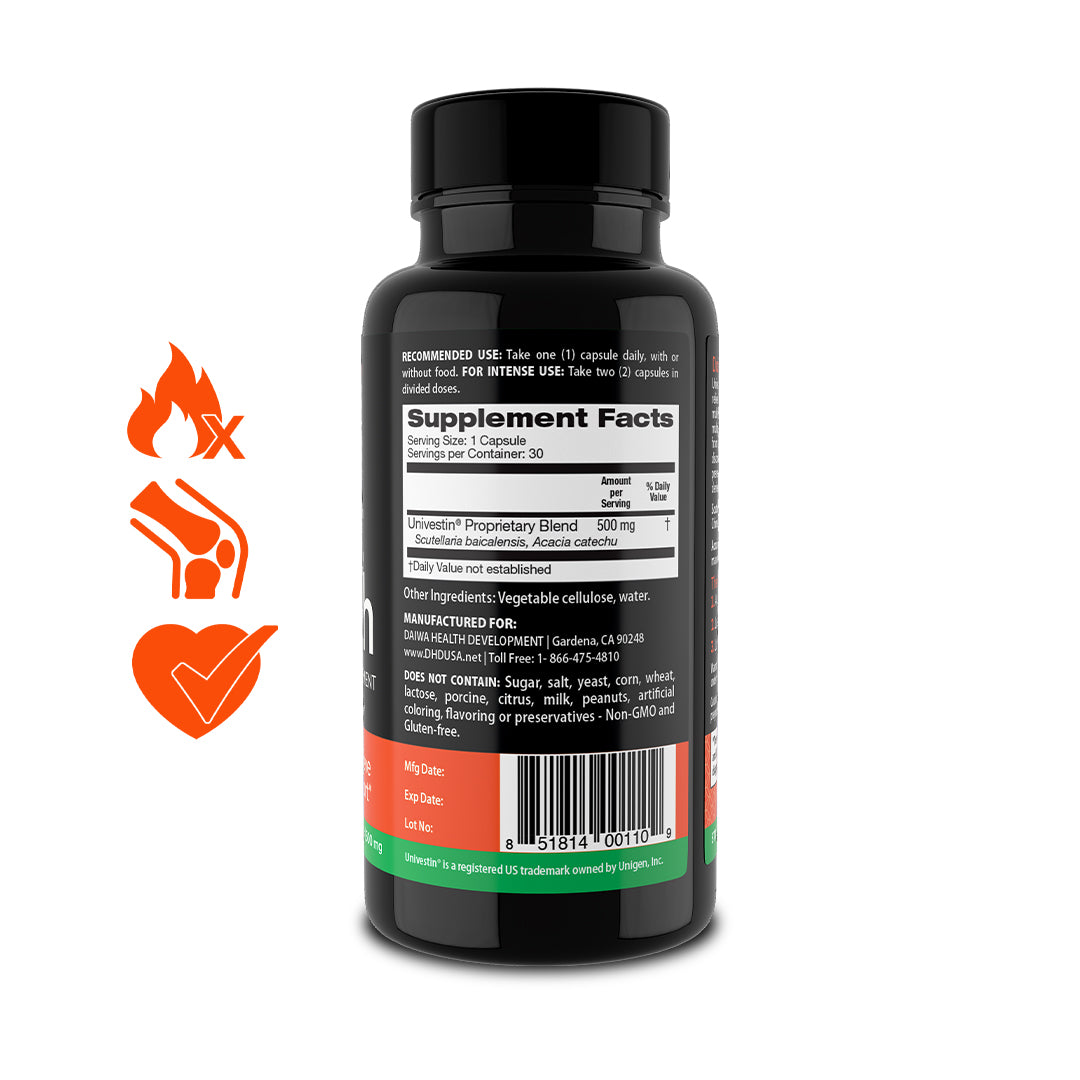
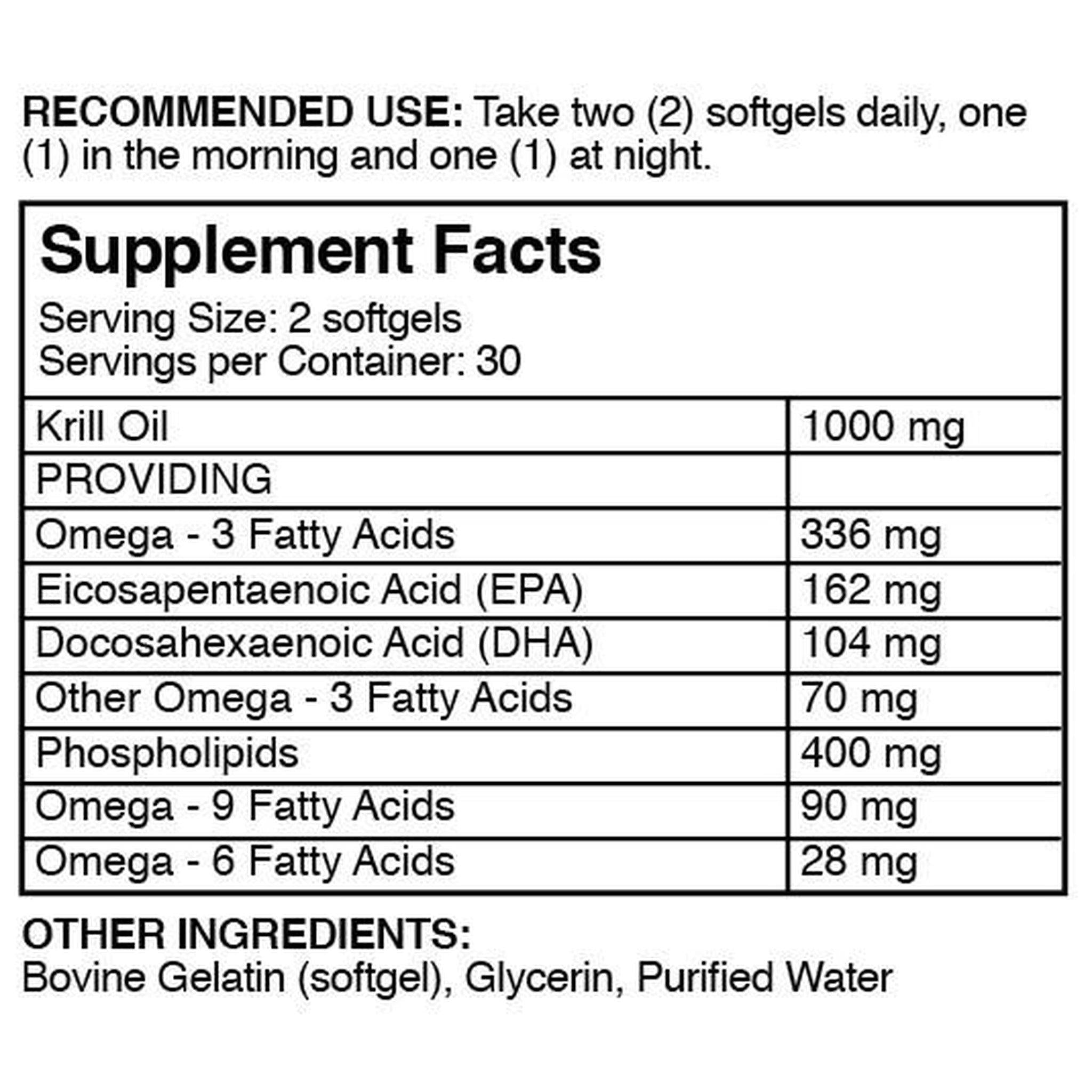
The Role of Supplements
Diet is the foundation, but supplements can help bridge the gap. At Daiwa Health Development, we design products that support the systems most affected by sodium—the heart, kidneys, and immune system.
When paired with a lower sodium diet, these supplements can:
-
Protect blood vessels from oxidative stress.
-
Support healthy blood pressure.
-
Manage the production of inflammatory cytokines.
-
Promote overall balance in the body.
Lifestyle changes aren’t always easy. That’s why having extra support can make the process smoother and more effective.
The Bigger Picture for Human Health
High salt intake is more than a personal habit—it’s a public health issue. Globally, excess sodium consumption contributes to nearly 3 million deaths every year. Rapid urbanization and reliance on processed foods are only driving the numbers higher.
For patients, the risks are immediate: higher blood pressure, increased risk of stroke, and more pressure on the kidneys. For healthcare systems, the burden is clear in rising rates of cardiovascular disease and related complications.
The evidence is overwhelming. Sodium doesn’t just change numbers on a lab report. It changes lives, sometimes in irreversible ways.
Finding Balance
The solution isn’t cutting salt completely—it’s about balance. The body needs sodium, but only in small amounts. By following dietary guidelines, focusing on low sodium intake, and pairing lifestyle choices with supportive supplements, patients can take back control of their health.
The path forward is simple but powerful: eat more whole foods, hydrate consistently, use movement to your advantage, and be mindful of how much salt is in your daily meals.
At Daiwa Health Development, we continue to build supplements backed by science to give people practical tools to manage sodium-related risks. With balance, awareness, and the right support, it’s possible to enjoy a longer, healthier life.