The Gut-Brain Connection: How Your Gut Health Affects Your Mental Health

Have you ever felt butterflies in your stomach before an important event or a gut wrenching sensation during a stressful day? These reactions are not coincidences. They are part of the scientifically established gut brain connection, an intricate communication network that links emotions, digestion, immunity, and even mental clarity. At Daiwa Health Development, we understand that strengthening this relationship is key to supporting long-term wellness through natural approaches and advanced supplements.
The guts, as a complex and neuron-rich system, play a crucial role in overall health by influencing brain function, immune response, and even the progression of diseases through the microbiome and enteric nervous system.
Understanding the Gut and Its Role in Health
The gastrointestinal tract (GI tract) is far more than a food-processing system. The gut breaks down nutrients, helps regulate digestion, absorbs energy, and influences the immune system, muscular system, and even bone health. When the digestive system is disrupted, the effects extend beyond digestion—showing up as fatigue, joint discomfort, or even altered mood.
This interaction is possible because the gut is often called the second brain, containing a dense network of over 100 million nerve cells in the enteric nervous system. This “neural network” operates semi-independently but communicates constantly with the brain, regulating gut motility, secretions, and immune cells that fight disease. The small intestine, with its specialized intestinal epithelium and diverse cell types, plays a crucial role in nutrient absorption, maintaining barrier integrity, and interacting with the microbiota to support gut homeostasis. The vagus nerve serves as the main link between the enteric nervous system and the brain, facilitating this critical communication.
The Brain: Central Command
The central nervous system, led by the brain, orchestrates thought, memory, breathing, heart rate, emotions, and stress response. Communication between our brains and the gut is bidirectional, forming the gut-brain axis, where signals travel both ways to influence mental and physical health. When the brain affects gut function, it influences everything from acid production and mucus secretion to the balance of gut microbes. For example, high stress levels can disrupt digestion, alter gut motility, and create gastrointestinal symptoms that feel like functional gastrointestinal disorders without an obvious physical cause.
The Enteric Nervous System: Your Second Brain
The enteric nervous system (ENS) is often called the “second brain” for good reason. This intricate network of over 100 million nerve cells is embedded throughout the walls of your gastrointestinal (GI) tract, orchestrating the complex processes that keep your gut working smoothly. Unlike any other part of the body, the ENS can operate independently of the central nervous system, managing gut motility, secretions, and blood flow on its own. Yet, it remains in constant communication with the brain through the vagus nerve, forming a vital part of the gut brain connection.
What makes the ENS remarkable is its ability to produce many of the same neurotransmitters as the brain, such as serotonin and dopamine, which are essential for both digestive and cognitive function. This neural network not only regulates digestion but also influences mood and mental clarity, highlighting the deep brain connection between the gut and the mind. A diverse gut microbiome is crucial for maintaining a healthy ENS, as imbalances can disrupt gut motility and have been linked to conditions like irritable bowel syndrome, anxiety, and depression. Understanding the ENS as your second brain underscores the importance of nurturing both your gut and your mind for optimal health.
The Gut-Brain Axis: Constant Communication
The gut brain axis describes the ongoing constant communication between brain and gut through pathways involving the vagus nerve, autonomic nervous system, enteric nervous system, and the hypothalamus-pituitary system. This axis ensures homeostasis and influences mental health, brain activity, and overall resilience. The vagus nerve also mediates various reflexes within the gut in response to changing conditions, further highlighting its role in maintaining balance. Practices like guided meditation can improve GI function by calming the vagus nerve and reducing stress, thereby supporting the gut-brain axis.
Research shows that disruptions in this axis may worsen functional bowel disorders, including irritable bowel syndrome (IBS) and chronic constipation. These conditions are examples of functional GI disorders, where symptoms exist without an obvious physical cause but are still deeply tied to gut brain communication. Irritable bowel syndrome (IBS) alone affects approximately 25-45 million people in the United States, underscoring the prevalence of these disorders.
The Role of the Vagus Nerve in Gut-Brain Communication
The vagus nerve is the main highway of the gut brain axis, carrying messages between the brain and gut in both directions. This powerful nerve helps regulate essential bodily functions, including digestion, heart rate, and even breathing. Through the vagus nerve, the brain can influence gut activity, while the gut can send signals back to the brain, shaping everything from mood to immune response.
One of the vagus nerve’s most fascinating roles is its impact on the gut microbiome. Changes in vagal tone can alter the composition and function of gut bacteria, which in turn can affect mental health and overall well-being. When the vagus nerve isn’t working properly, it can contribute to gastrointestinal disorders like irritable bowel syndrome, functional dyspepsia, and GERD. Research also shows that vagus nerve dysfunction is linked to mental health disorders such as anxiety and depression, further emphasizing the importance of the gut brain connection. Supporting vagus nerve health is a key step in maintaining a balanced gut, a resilient mind, and overall health.
The Gut Microbiome: Tiny Organisms, Big Impact
Trillions of microorganisms—known collectively as the gut microbiome—reside in the gut and send chemical messages that directly affect the brain connection. A diverse gut microbiome supports digestion, nutrient absorption, and even cognitive function. The gut microbiome also produces neurotransmitters such as serotonin, which influence mood and physiological functions. Animal experiments, including research on germ free mice, demonstrate that without these microbes, the nervous system and motor function of the gut and brain develop abnormally.
When gut bacteria are imbalanced, it can impair the blood brain barrier, influence brain hormones, and increase risk for mental health disorders such as anxiety, depression, and even neurodevelopmental disorders like autism spectrum disorder. Findings suggest that improving overall gut health can reduce symptoms of gastrointestinal problems and improve mental health outcomes. Most of the body's serotonin is produced and stored in gut cells, playing a vital role in maintaining gut and brain health.
Brain and Gut: Similarities and Differences
While the brain and gut may seem worlds apart, they share surprising similarities that are central to the gut brain axis. Both organs are packed with complex networks of nerve cells and produce many of the same neurotransmitters, allowing them to communicate efficiently through the vagus nerve. This constant exchange of information enables the gut and brain to influence each other’s function, from digestion to mood regulation.
Despite these connections, the brain and gut also have distinct roles. The brain is the command center for movement, sensation, and higher cognitive functions, while the gut specializes in breaking down food, absorbing nutrients, and eliminating waste. Their structures and responses to stimuli differ as well, with the gut’s enteric nervous system capable of operating independently, unlike any other organ system. Appreciating both the similarities and differences between the brain and gut helps us understand why the gut brain connection is so vital for overall health and well-being.
How the Brain Affects the Gut
Just as gut microbes influence the brain, the brain affects gut function through stress signaling. Heightened stress levels activate the autonomic nervous system, which alters gut motility, acid secretion, and protective mucus. These shifts can worsen gut issues or aggravate gastrointestinal symptoms. Over time, unmanaged stress may trigger anxiety like behaviors, gut feelings of discomfort, and contribute to functional bowel disorders. Consuming too many processed foods can also disrupt gut health and impair the gut-brain connection, further exacerbating gut issues.
Gastrointestinal Problems and the Gut-Brain Connection
Gastrointestinal problems like irritable bowel syndrome, inflammatory bowel disease, and other functional gastrointestinal disorders are more than just digestive issues—they are deeply intertwined with the gut brain connection. These conditions often present with chronic symptoms such as abdominal pain, bloating, and irregular bowel habits, which can be triggered or worsened by disruptions in gut brain communication, gut motility, and the gut microbiome.
Psychological factors, including stress and anxiety, can intensify GI symptoms, creating a cycle that affects both the gut and the brain. That’s why a comprehensive treatment plan for GI problems often includes not just dietary changes, but also stress management and psychological therapies like cognitive-behavioral therapy (CBT) and gut-directed hypnotherapy. By addressing both the physical and emotional aspects of gut health, it’s possible to reduce symptoms and to improve quality of life, highlighting the importance of a holistic approach to the brain connection in digestive health.
Resetting the Gut-Brain Connection
Healing the gut and brain relationship requires a comprehensive treatment plan supported by both lifestyle and nutritional interventions.
Supporting Gut Health
- Fiber-rich foods (spinach, carrots, beetroot, sweet potatoes) encourage healthy gut working by feeding beneficial microbes.
- Fermented foods like yogurt, kefir, and kimchi deliver live bacteria that strengthen the microbiome.
- Pre/pro/post biotic supplements, such as those developed at Daiwa Health Development, help restore microbial balance and protect against gastrointestinal problems.
Supporting Brain Health
- Adequate sleep strengthens memory and clears metabolic waste from the brain.
- A balanced diet, particularly the Mediterranean diet, slows cognitive decline and supports neurological health.
- Mentally stimulating activities improve cognitive function and safeguard against brain disorders like Alzheimer’s disease.
Pro Tip:
A 30 day gut reset focusing on a balanced diet, regular exercise, and targeted pre/pro/post biotics can significantly improve overall gut health while reducing the burden of functional GI disorders.
The Emotional and Physical Connection
Unresolved stress, early life stress, or high anxiety can create gut-driven changes in mood and increase risk for mental health disorders. At the same time, a poorly functioning GI tract can worsen depression or influence mood through changes in the microbiome. This bidirectional relationship explains why healthcare providers now treat gut brain connection issues with an integrated focus—balancing both brain health and gut health in order to improve physical health.
The Future of Gut-Brain Research
The field of gut brain axis research is advancing rapidly, opening new doors for understanding and treating both GI problems and mental health disorders. Scientists are exploring innovative therapies such as psychobiotics, prebiotics, and probiotics that target the gut microbiome to support mental health and brain function. There is also growing interest in how the gut brain connection influences neurological and psychiatric conditions, including autism spectrum disorder, Alzheimer’s disease, and Parkinson’s disease.
Cutting-edge technologies like functional MRI and machine learning are helping researchers map the intricate brain connection with the gut in unprecedented detail. These advances promise to pave the way for personalized treatment plans that address the unique needs of each individual, improving outcomes for both gut and brain health. As our understanding of the gut brain connection deepens, the future holds exciting possibilities for enhancing overall health and quality of life through targeted, science-backed interventions.
Putting It All Together
The gut brain relationship is not just theory—it is daily reality, shaping how you think, feel, and function. From gut motility and motor function to memory and brain function, this connection is powerful, personal, and deeply tied to wellness. Functional medicine emphasizes that supporting both the brain and the gut simultaneously leads to more lasting results than treating them separately.
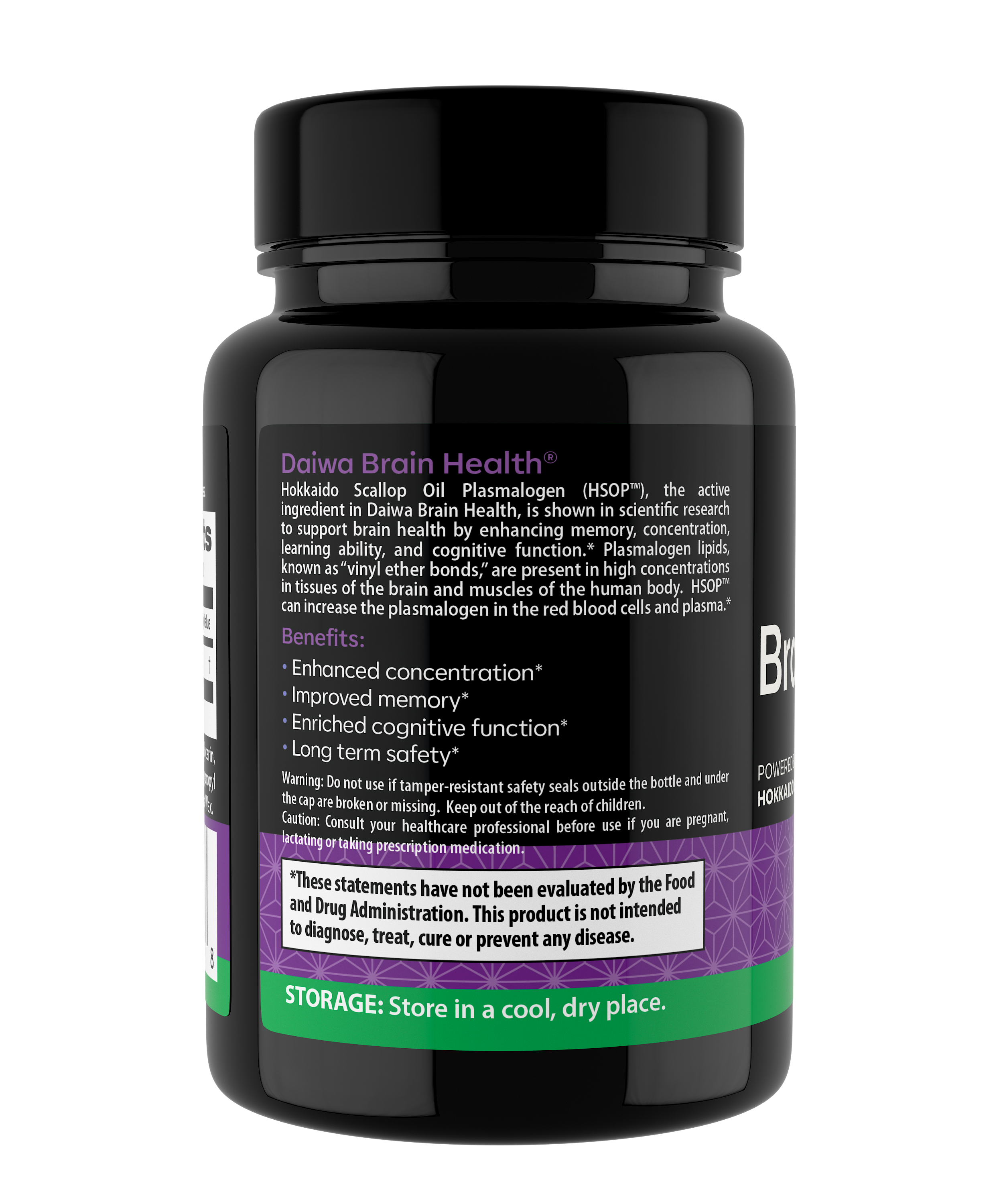
At Daiwa Health Development, our mission is to provide supplements that strengthen this vital system, reduce gastrointestinal symptoms, and support long-term overall health. By focusing on the gut brain connection, we give you tools to restore balance, build resilience, and thrive.
In summary: The brain and gut connection impacts not only digestion but also mental health, immunity, and longevity. A strong, diverse gut microbiome, supported by lifestyle changes and targeted supplementation, improves quality of life while reducing the risk of functional bowel disorders, brain disorders, and mental health disorders. When both systems are aligned, the entire body benefits.
Daiwa Health Development proudly delivers products designed to strengthen this connection—because when the gut and brain work together, optimal health follows.