Antibiotics have saved millions of lives since their discovery. They stop dangerous bacterial infections, cure pneumonia, and prevent complications from wounds that once proved fatal. Yet, while their benefits are undeniable, so are their side effects.
The effects of antibiotics on gut microbiota are significant, antibiotic treatment can reduce gut microbiota diversity, alter the gut ecosystem, and promote antibiotic resistance, leading to metabolic changes and long-term consequences for gut health.
At Daiwa Health Development, we’ve seen how antibiotic treatment can disrupt the body’s most intricate ecosystem: the gut microbiome. These medications don’t distinguish between harmful invaders and the beneficial bacteria that keep digestion, immunity, and mood in balance. Maintaining gut microbiota diversity is crucial for a healthy digestive tract and overall well-being. The result can be lasting changes to the gut microbiota - and ultimately, your overall well-being.
This article examines the effects of antibiotics on gut health, what happens inside the gut during and after antibiotic use, and how you can restore microbial harmony through diet, lifestyle, and supplementation. The digestive tract is the primary site where these changes take place.
Why Antibiotics Are Both Lifesaving and Disruptive
Antibiotics are powerful tools for treating bacterial infections. They target specific bacterial species or groups, halting their growth or killing them outright. Penicillin, the first antibiotic, revolutionized medicine, and modern antibiotics continue to save lives from urinary tract infections, respiratory diseases, and other infectious diseases.

However, the human gut contains more than 100 trillion microbes, collectively known as the human gut microbiota - that support digestion, synthesize vitamins, and protect against pathogenic bacteria. This ecosystem has the highest species diversity and quantity of microorganisms in the body. Antibiotics, even short courses, can disturb this balance by wiping out large populations of gut bacteria and affecting the overall microbial composition, which can influence health outcomes such as obesity, immune development, and disease susceptibility.
The outcome depends on factors such as the antibiotic type, dosage, and duration of antibiotic therapy. Some antibiotics, like clindamycin or broad-spectrum penicillins, can drastically alter the gut microbiota composition in just a few days, impacting not only the targeted bacteria but also other bacteria that are part of the diverse microbial community.
Antibiotic Administration and Use
Antibiotic administration remains a cornerstone in treating bacterial infections, offering rapid relief and preventing complications from illnesses that once posed serious threats to human health. When prescribed appropriately, antibiotics can be lifesaving, targeting harmful bacteria and helping the body recover from infections such as strep throat, urinary tract infections, and other common bacterial diseases.
However, every course of antibiotics has a ripple effect on the gut microbiome. These powerful medications do not discriminate between pathogenic bacteria and the beneficial microbes that support gut health. As a result, even short-term antibiotic use can disrupt the delicate balance of the gut microbiome, sometimes leading to digestive discomfort, reduced microbial diversity, and a weakened immune response.
Responsible antibiotic administration is essential, not only for effective treatment of bacterial infections but also for preserving the long-term health of the gut. Overuse or misuse of antibiotics can accelerate the development of antibiotic resistance, making it harder to treat infections in the future. When bacteria in the gut are repeatedly exposed to antibiotics, they can develop resistance, and these antibiotic resistant strains may spread within the body and to others.
To protect your gut health and help combat antibiotic resistance, it’s important to use antibiotics only when truly necessary and always as directed by a healthcare professional. This careful approach ensures that antibiotics remain effective for treating bacterial infections, while minimizing their impact on the gut microbiome and reducing the risk of antibiotic resistance for everyone.
The Gut Microbiome: A Complex Microbial Community
The gut microbiome is one of the most complex ecosystems in the human body. It includes bacteria, fungi, viruses, and archaea, all living symbiotically within the gastrointestinal tract. These diverse microbial communities, often referred to as gut microbiomes, play a crucial role in maintaining digestive health.
When balanced, this complex microbial community - also known as the enteric microbiota - produces short chain fatty acids (SCFAs) that feed colon cells, regulate inflammation, and maintain the gut barrier. But when disrupted, the gut microbiota loses diversity, weakening the immune defense and allowing harmful bacteria to thrive.
Key Functions of the Gut Microbiome
- Digestive System Support – Breaks down fibers, complex carbohydrates, and bile acid metabolism products for nutrient absorption.
- Immune System Regulation – Gut microbes communicate with the intestinal immune system, supporting immune functions by promoting tolerance to beneficial microbes and defending against pathogens.
- Mental Health Balance – Through the gut brain axis, microbes influence neurotransmitter production, affecting stress, anxiety, and mood.
- Protection from Disease – A strong gut microbiota and its gut microbes prevent colonization by enteric pathogens such as Escherichia coli and Clostridium difficile (C. Difficile).
What Happens to the Gut During Antibiotic Treatment
During antibiotic administration, both good and bad bacteria are exposed. The medication kills sensitive strains while resistant or dormant microbes survive. Common gastrointestinal issues due to antibiotics include diarrhea, cramping, and bloating.
1. Loss of Microbial Diversity
The human gut microbiome loses richness, meaning fewer microbial communities survive. This imbalance makes it easier for pathogenic bacteria to overgrow, leading to antibiotic associated diarrhea or yeast overgrowth.
2. Decrease in Short Chain Fatty Acids
Antibiotics suppress the production of short chain fatty acids by wiping out the microbes that produce them. This constraint reduces energy for intestinal cells, weakens the gut barrier, and triggers intestinal inflammation.
3. Weakened Immune Function
A disturbed gut microbiota limits immune responses, making the body more prone to new bacterial infections and viral illnesses.
The gut microbiota also matters in maintaining intestinal immunity by supporting immune defenses in the gut, and disruption can impair these protective functions.
4. Overgrowth of Clostridium Difficile
Perhaps the most dangerous consequence is Clostridium difficile infection (CDI). When antibiotic therapy eliminates protective bacteria, C. Difficile spores can take over, causing severe diarrhea, fever, and intestinal inflammation. In some cases, CDI becomes chronic or leads to refractory Clostridium difficile infection that requires advanced treatment such as fecal microbiota transplantation.
Antibiotic Associated Diarrhea: A Common Side Effect
Antibiotic associated diarrhea (AAD) affects up to 30% of patients after antibiotic use. It occurs when the balance between beneficial bacteria and harmful bacteria in the digestive system shifts toward the latter.
While mild AAD resolves naturally, recurrent or severe cases signal a loss of microbial protection. In such situations, probiotic supplementation and fermented foods can help restore equilibrium and prevent C. Difficile disorders.
For more details, see The benefits of a high-fiber diet for gut health. For more details, see Daiwa Brain Health®. For more details, see PeakImmune4® Ultra 500mg. For more details, see gut health supplements. For more details, see DAIWA GASTROIMMUNE™.Go Beyond Probiotics for Gut Health
If your gut lining is compromised, adding more bacteria doesn't fix the structural problem. Daiwa Gastro Health uses patented IGY Max® immunoglobulin technology to support the gut barrier itself, the wall that determines what enters your bloodstream.
Learn MoreAntibiotic Resistance: A Growing Global Concern
Repeated and unnecessary antibiotic use contributes to antibiotic resistance - a condition where bacteria evolve to survive drug exposure. These antibiotic resistant bacteria make standard treatments less effective and increase the risk of persistent infections. Increased antibiotic use has been linked to the global antibiotic resistance crisis.
Within the human gut, overuse of antibiotics can lead to the accumulation of antibiotic resistance genes (ARGs). These genes can transfer between species, spreading bacterial antibiotic resistance across populations.
Even low doses of antibiotic exposure - for instance, through livestock or food residues, may encourage this resistance, making future antibiotic treatment more complicated.
The Long-Term Effects of Antibiotics on Gut Health
The effects of antibiotics on gut health can last weeks, months, or even years depending on microbial recovery and overall human health. Disrupting the gut microbiota can have negative effects, such as increasing the risk of metabolic disorders and reducing the effectiveness of probiotics.
- Reduced Microbial Diversity – Fewer bacterial species mean fewer nutrients, enzymes, and immune messengers produced in the gut, impacting the balance of the intestinal microbiota.
- Intestinal Inflammation – Loss of beneficial gut bacteria increases permeability and allows toxins to cross the gut wall, resulting in intestinal inflammation or inflammatory bowel disease.
- Impaired Bile Acid Balance – Antibiotics alter primary bile acids and secondary bile acids, affecting digestion and bile acid metabolism.
- Weakened Immune Function – The immune system relies on signals from gut microbiota functions; their absence impairs defense mechanisms.
- Mental Health Impact – Disrupted gut brain axis signaling can contribute to anxiety, low mood, and cognitive fog.
Dysbiosis can impair the immune system, reduce the production of beneficial short-chain fatty acids, increase susceptibility to opportunistic infections, and potentially contribute to long-term metabolic and immune-related conditions by disturbing the intestinal microbiota.
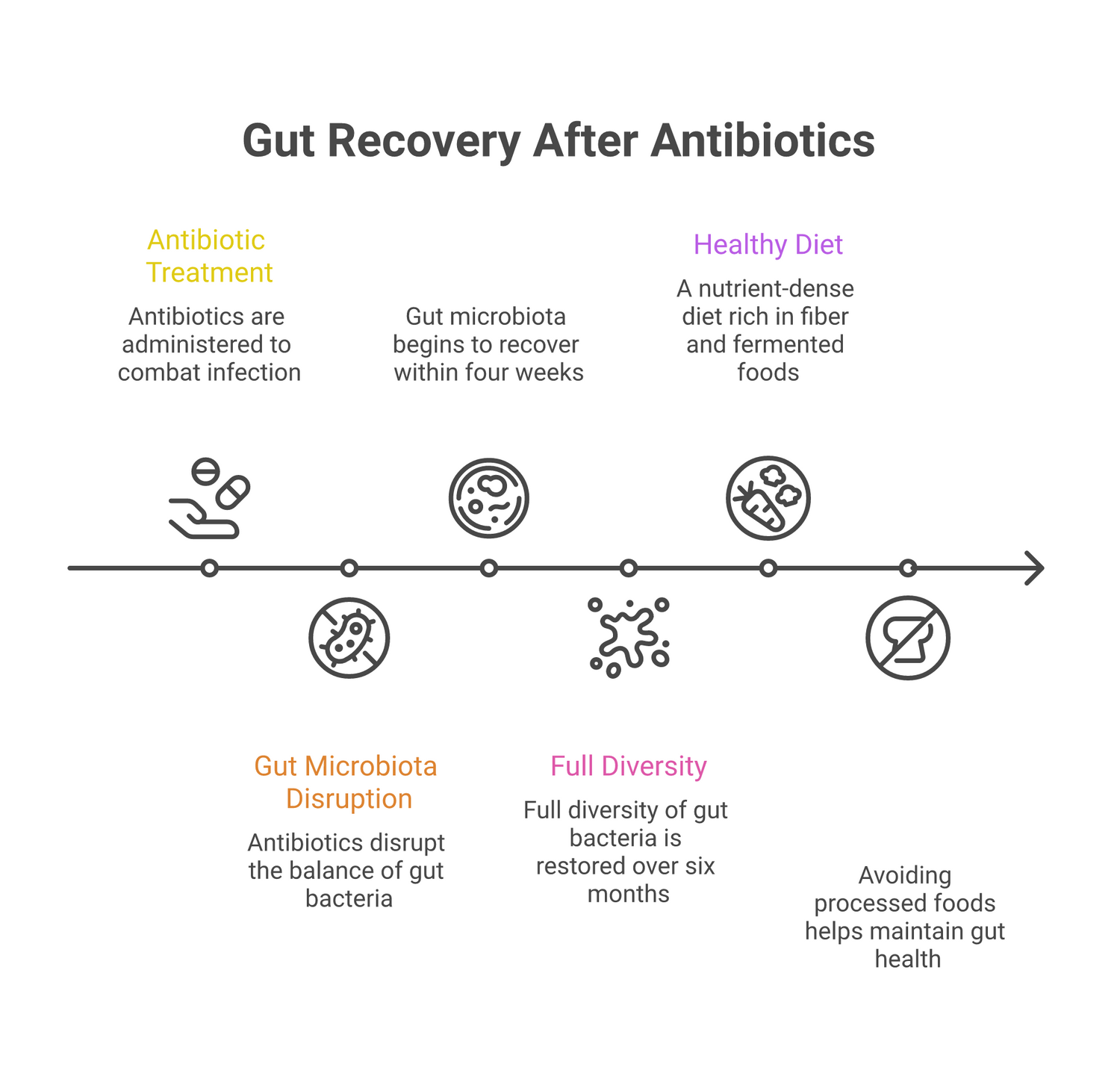
How Long Does It Take the Gut to Recover After Antibiotics?
Recovery time varies. Some research shows partial restoration of the gut microbiota within four weeks, but full diversity can take six months or more. Factors include:
- Type and duration of antibiotic therapy
- Age and general health
- Diet quality and fiber intake
- Exposure to fermented foods or probiotic strains
A nutrient-dense, healthy diet rich in plant fibers and fermented foods helps accelerate recovery. Avoiding processed foods and focusing on whole grains, vegetables, and healthy fats gives the human gut the building blocks it needs to rebuild.
How to Reset Your Gut Bacteria After Antibiotics
Restoring healthy gut bacteria takes time, consistency, and supportive nutrition. The following strategies help repair microbial balance after antibiotic use:
1. Eat Fiber-Rich Foods
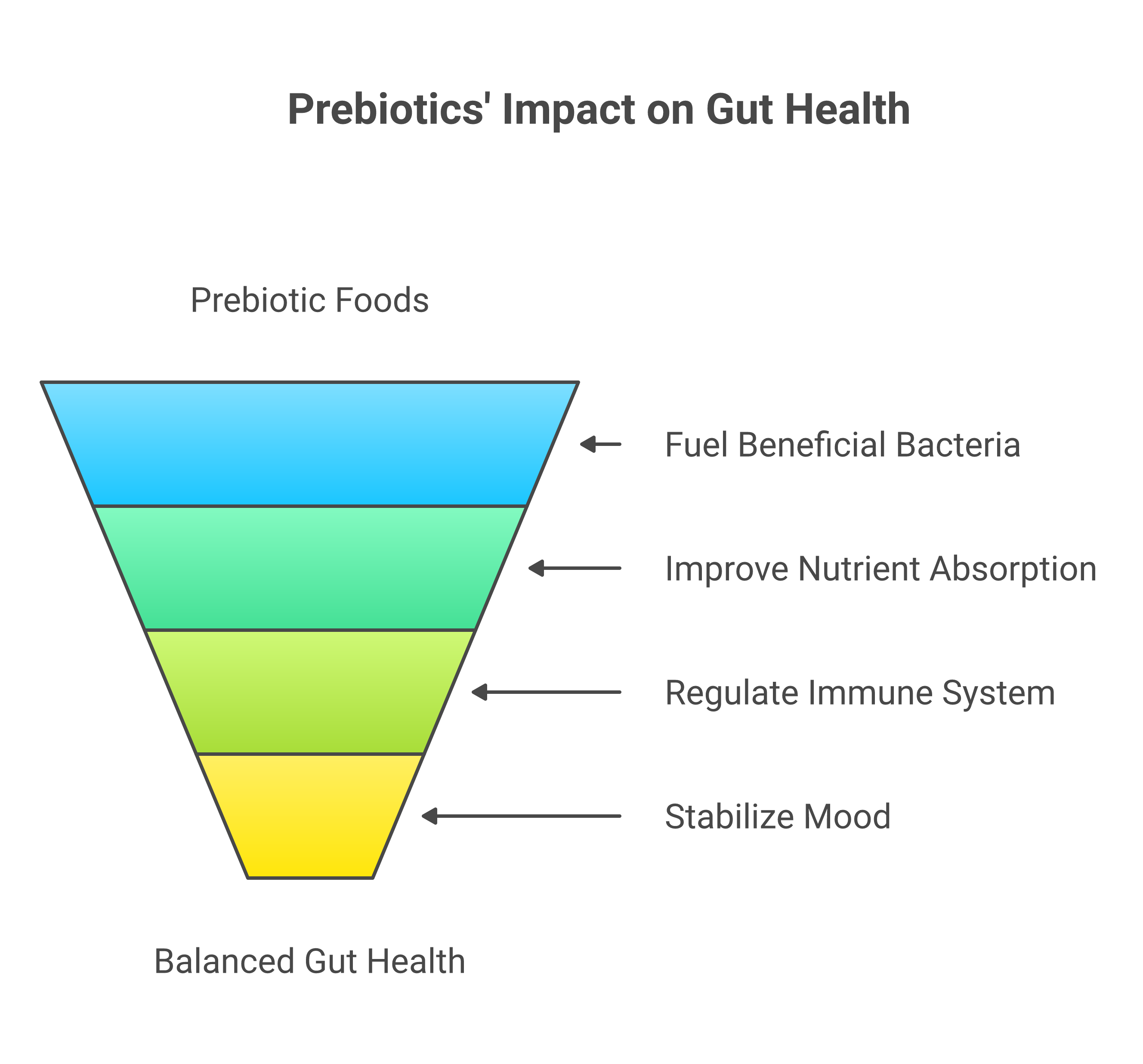
Prebiotic fibers in vegetables, fruits, and legumes feed beneficial bacteria and promote SCFA production. This diet manages intestinal inflammation and strengthens the gut lining.
2. Include Fermented Foods
Foods like yogurt, kefir, kimchi, and sauerkraut reintroduce live probiotic strains that enhance gut microbiota recovery.
3. Take Probiotics Wisely
After antibiotic treatment, consider probiotic supplements containing strains such as Lactobacillus rhamnosus and Saccharomyces boulardii. These probiotic ingredients can reduce antibiotic associated diarrhoea and help replenish the gut flora.
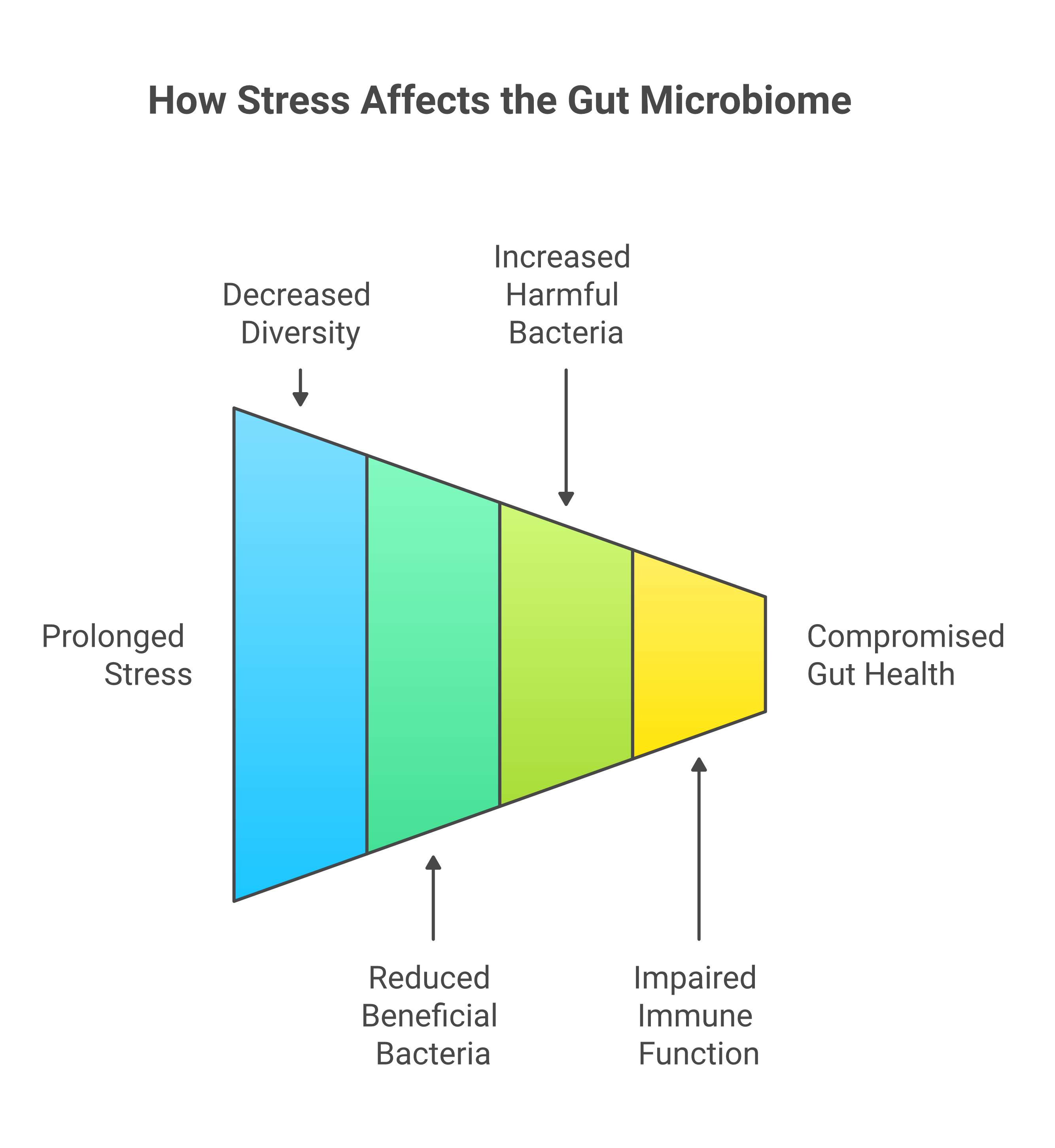
4. Manage Stress
High stress can suppress microbial regrowth and alter gut microbiota composition. Techniques like meditation, gentle exercise, and deep breathing support immune system and digestion.
5. Avoid Additional Antibiotic Exposure
Only take antibiotics when prescribed and necessary. Repeated antibiotic administration before full recovery delays microbial restoration and increases resistance.
Do You Need to Take Probiotics After Antibiotics?
While not every case requires supplementation, probiotic strains can make a measurable difference after antibiotic therapy. Clinical trials show they lower the risk of antibiotic associated diarrhea and promote a faster return to healthy gut bacteria.
At Daiwa Health Development, we recommend pairing probiotics with fermented foods and prebiotics to support natural recolonization. This three-part approach, probiotic intake, fiber feeding, and nutrient support, enhances the gut microbiota’s ability to recover fully.
Antibiotic Exposure in Early Life and Long-Term Health
Early antibiotic exposure in infancy can have lifelong effects. The human gut microbiota is still forming during the first three years of life, and antibiotics at this stage may alter its development. Studies link early exposure to increased risks of obesity, metabolic syndrome, and allergies later in life. Additionally, exposure to antibiotics in infancy is linked to increased lifetime risk of infections, asthma, obesity, inflammatory bowel disease, and neurodevelopmental disorders.
Parents should discuss alternatives with healthcare providers when possible and use antibiotic therapy judiciously to protect long-term human health.
Preventing Antibiotic-Associated Yeast Infections
When antibiotic use reduces protective bacteria, fungi like Candida can multiply, leading to yeast infections. This imbalance can occur in the mouth, intestines, or reproductive tract.
Preventive steps include maintaining beneficial bacteria through diet and probiotics, minimizing sugar intake, and wearing breathable fabrics to discourage fungal growth.
The Role of the Immune System
The immune system relies heavily on signals from the gut microbiota. When antibiotics disturb this relationship, immune defenses weaken.
The gut microbiota also helps regulate the production of antimicrobial peptides, which are secreted by intestinal epithelial cells and play a crucial role in gut mucosal immunity by controlling gut bacteria and maintaining the epithelial barrier.
A healthy microbiome encourages the development of regulatory T cells that prevent excessive inflammatory responses. After antibiotic exposure, these mechanisms falter, leaving the body more prone to illness.
Supporting immunity means supporting the microbiome, with balanced nutrition, sufficient rest, and strategic supplementation.
When Antibiotic Resistance Spreads
The effects of antibiotics extend beyond one person’s gut. Wastewater, agriculture, and global travel have turned antibiotic resistance genes into a shared environmental issue.
Resistance genes from the human gut can transfer to soil microbes, spreading antibiotic resistant bacteria worldwide. Reducing overuse, choosing targeted antibiotic treatment, and supporting gut recovery help slow this cycle.
Bile Acids, Metabolism, and Gut Recovery
The gut microbiota regulates bile acid metabolism, transforming primary bile acids into secondary bile acids that aid digestion and lipid absorption. After antibiotics, this process becomes impaired, leading to fat malabsorption and altered metabolism.
Reintroducing fermented foods, probiotics, and fibers helps restore bile acid processing, improve lipid balance, and reduce digestive distress.
Modern Research and the Human Gut Microbiome
Recent research by Zhao et al., Smith et al., and Nguyen et al. (2021-2024) reveals just how critical microbial diversity is for recovery after antibiotic therapy. Findings show that individuals with diets rich in fiber and fermented foods regained microbial diversity up to 50% faster than those eating processed foods.
Animal model studies on the murine colonic microbiome have provided valuable insights into how antibiotics affect gut microbial communities and the process of recovery, helping researchers better understand microbiota dynamics and responses to interventions.
Another study by Lee et al. Found that resistant microbial strains persisted for months after antibiotic exposure, carrying resistance genes linked to immune dysregulation and inflammatory bowel disease.
These studies highlight why dietary care, stress management, and probiotic support are essential for restoring the human gut microbiome post-treatment.
Daiwa Health Development’s Role in Gut Restoration
At Daiwa Health Development, our mission is to bridge science and wellness. We understand how fragile the microbiome becomes after antibiotic treatment - and how critical it is to restore microbial diversity safely.
Our supplements are designed to protect and rebuild the gut microbiota, encouraging beneficial gut bacteria to flourish while supporting immune recovery. By combining probiotic cultures with prebiotic fibers and our formulas promote gut health and balance after antibiotic exposure.
The Path to a Healthy Gut After Antibiotics
Healing the human gut after antibiotic use requires time, patience, and consistency. Here’s how to support a complete reset:
- Eat Whole Foods: Focus on vegetables, fruits, and whole grains to nourish the microbiome.
- Incorporate Fermented Foods: Replenish good bacteria naturally.
- Supplement Wisely: Use scientifically backed probiotics and prebiotics.
- Avoid Processed Foods: Minimize sugar and additives that feed harmful bacteria.
- Stay Active: Movement supports digestion and blood flow.
- Sleep and Hydrate: Both are essential for microbial repair and detoxification.
★★★★★ Trusted by thousands of customers
Ready to Fix the Root Cause of Gut Issues?
Daiwa Gastro Health addresses what most gut supplements ignore: the integrity of the gut lining. Powered by patented IGY Max® technology, it supports the barrier that determines what enters your bloodstream and what doesn't.
Shop Daiwa Gastro HealthFree shipping on orders over $50 · 30-day guarantee
Conclusion: A New Understanding of Gut Health
Antibiotics remain one of medicine’s greatest achievements. But we now understand that every dose has ripple effects inside the body. The effects of antibiotics on gut health extend beyond the digestive system, influencing metabolism, immunity, and even mental well-being.
Fortunately, the gut is resilient. With mindful nutrition, fermented foods, probiotic strains, and the right lifestyle choices, the human gut microbiota can recover, rebuild, and protect you for years to come.
At Daiwa Health Development, we’re proud to support this recovery process with evidence-based solutions designed to strengthen microbial health, defend the immune system, and restore harmony after antibiotic therapy.
Your microbiome is your greatest ally, protect it, feed it, and it will protect you in return.





Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.